
.
.

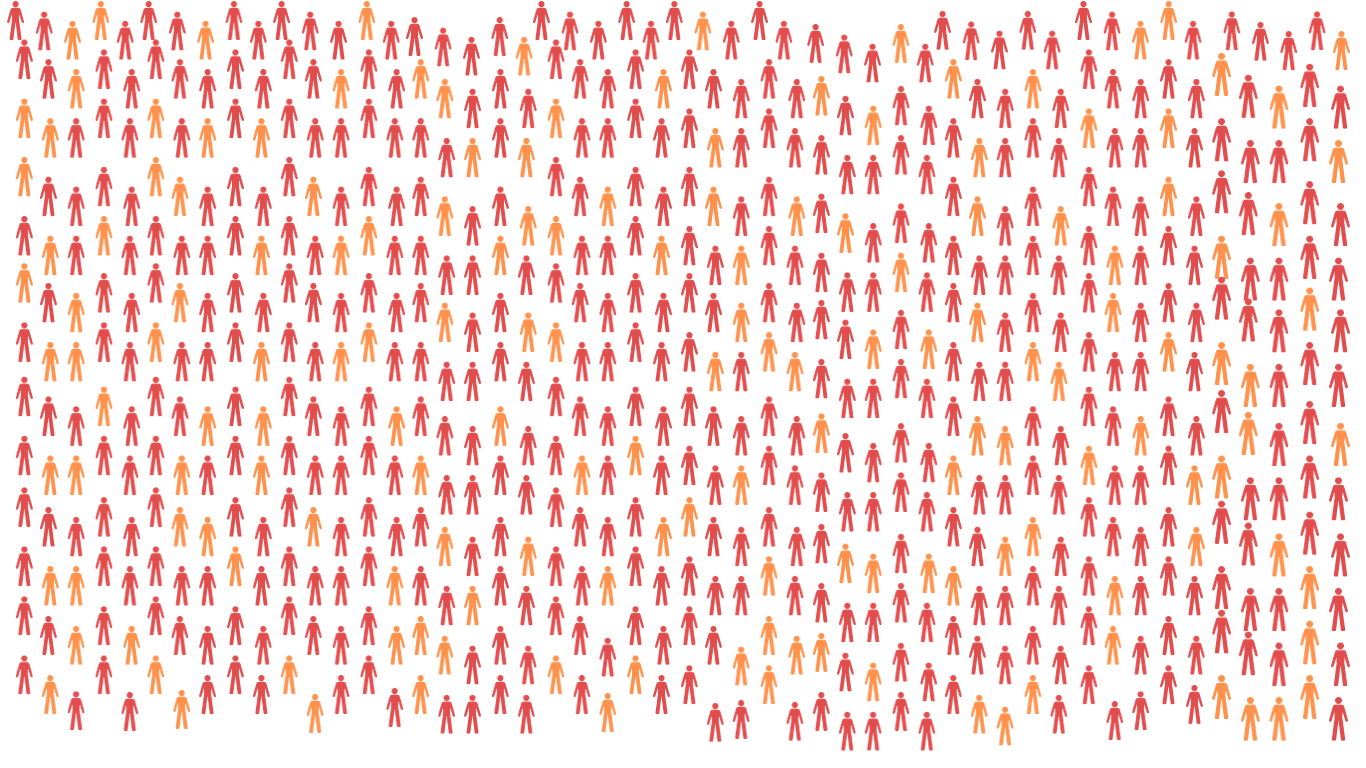
Over 250,000 people have ME in the UK. [1]
Scroll down.
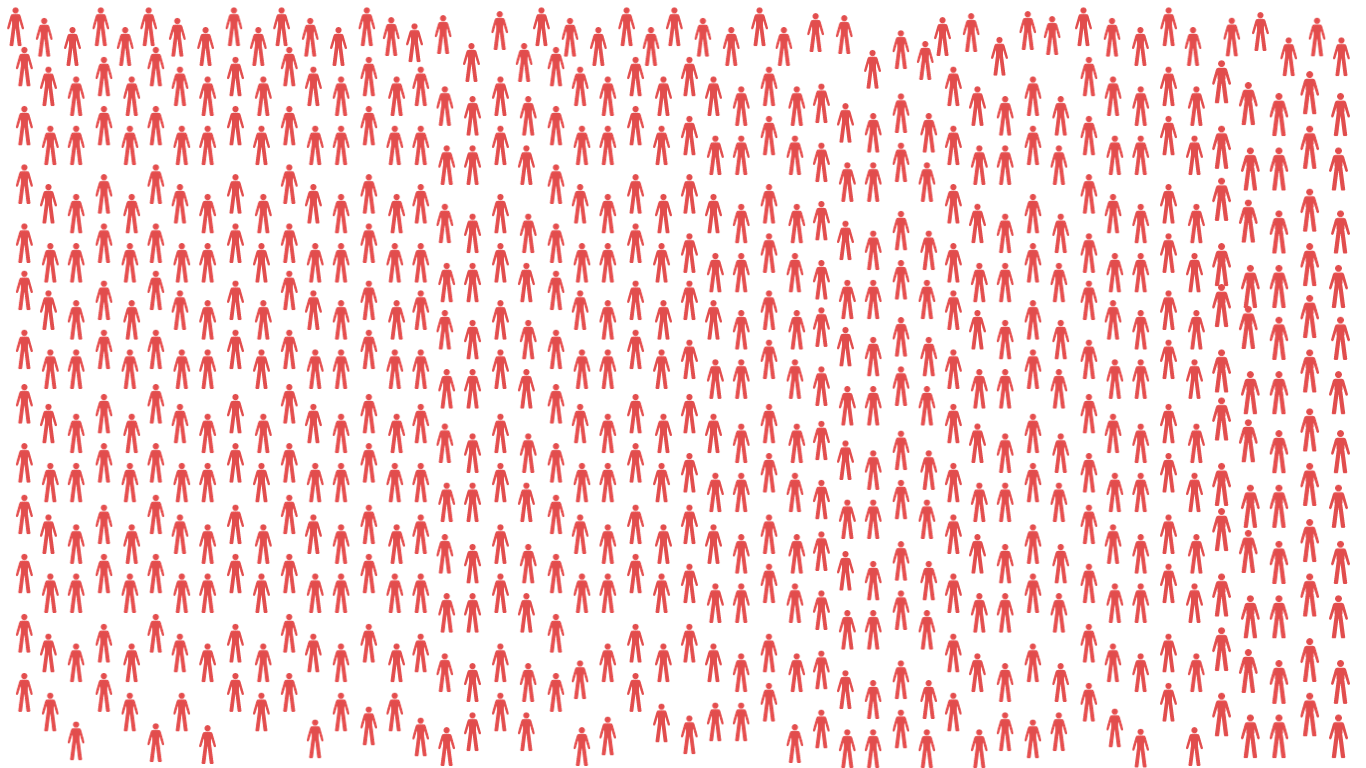
This is 1 in every 263 people. [2]
Each icon represents a person living with ME in the UK.
ME is a debilitating, multi-system condition affecting a person’s neurological, immunological, endocrine and musculoskeletal systems. [3]
We do not know what causes it.
We do know that the quality of life of ME is lower than conditions such as multiple sclerosis and cancer. [3][4][5]
27% of people with ME live with daily extreme pain. [4]

25% of people with ME are bedbound or housebound. [3]
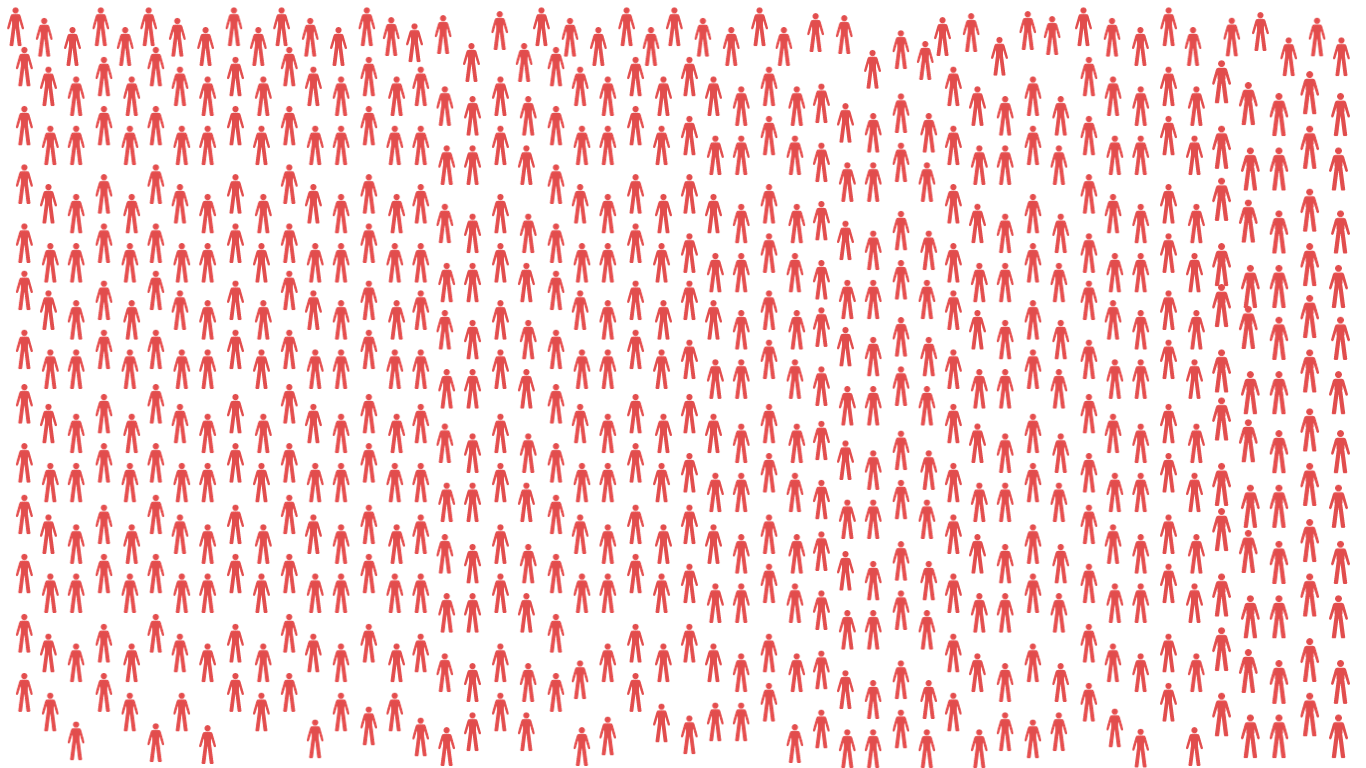
Each orange icon represents one of the 62,500 with severe ME.
Severe ME can be terrifying. It can include:
Musculoskeletal weakness and muscle wastage [6]
Reduction in blood to the brain [7]
Life threatening malnutrition [8]
Paralysis [9]
Atypical seizures [9]
Severe noise and light sensitivity [9]

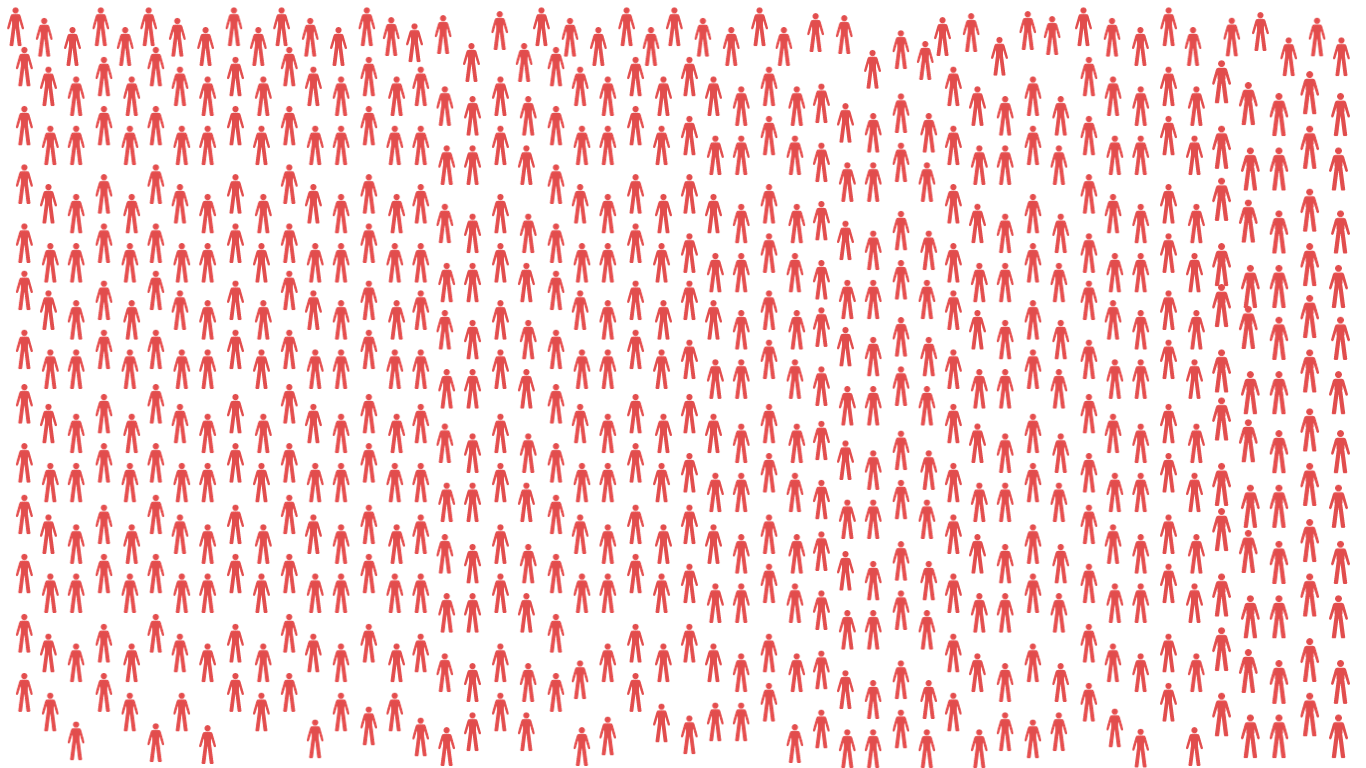
Among those with moderate and severe ME, 57% have seriously contemplated suicide. [10]
Each blue icon represents someone in this 57%.

Sit with this number for a moment.
Think about the scale of suffering.

Whilst the number of people with ME is devastating, it is just the tip of the iceberg.

The way we treat people with ME is unfathomably cruel.

We call them liars. [12]
Medical professionals refer to ME as ‘Multiple Excuses’. [13]
People with ME are blamed for wasting doctors time and are told they are making it up. [14] [15]

We falsely claim ME is psychological, not physiological. [16]
People with ME are treated like their belief that they are ill is what is making them sick. [17]
They are told that their illness is ‘fear-based’. [16][17]

But people with ME are not liars, nor is ME psychological. [16][18]
It is neurological. [19][20][21]
It is immunological. [19][21]
It is muscular. [22][23]
It deregulates the heart, blood and circulation. [24][25][26][27][28][29][30]
It deregulates the gastrointestinal system and metabolism. [31][32][33][34][35][36][37][38]

We have known that ME is neurological since the 1960’s. [11]
Yet we still blame patients for making it up, or for
causing their illness with their own ‘negative belief’. [17]

Blaming people with ME, or attributing it to psychology causes phenomenal harm.

It puts families through hell.
The families of 1 in 5 children with ME are wrongfully
referred to child protection proceedings. [11]

It impacts the funding of research.
Government funding for ME research stands at £1 for every sufferer.
This is far less than neurological conditions of similar prevalence. [11]
Of the research that is funded the focus is on behavioural studies, rather than on finding a biological cause or cure. [11]

Without this funding, there will never be a cure.

Blaming people with ME is not the only way we fail them.

We fail to diagnose.
For those that are lucky to be diagnosed, it often takes years.
For 19% of people with ME, this diagnosis will take more than half a decade. [39]

We fail to provide basic medical services.
There is a lack of specialists throughout the country
and entire regions do not have secondary services at all. [11]
This lack of services has been referred to as a humanitarian crisis. [40]

We fail to educate doctors.
In the UK, some GPs do not recognise the condition. [14]
Many primary care professionals do not receive training on ME. [11]

Take a moment to imagine living with ME.
You have a neurological condition that impacts your ability to perform daily tasks.

You become too disabled to leave your house.
You have fatigue, memory loss and extreme muscle weakness.
You cannot support your own body weight.
Even eating and bathing becomes difficult. What next?

Now imagine that you have been told you are just being lazy.
Your friends tell you ‘we all get tired’.
You are told you are lucky you get to stay home all day.
People don’t think it is serious. How alone do you feel?

Imagine that your doctor doesn’t take ME seriously either.
It takes years to be diagnosed.
Even then, your doctor thinks ME is basically attention seeking anyway.
You can’t go to your doctor without being blamed. How do you ask for help?

Imagine trying to manage the symptoms alone.
The illness is a daily struggle.
You struggle to walk, go to the toilet, or hold a conversation.
You might have atypical seizures. You cannot tolerate sound. How do you cope?

Imagine that the DWP refuses your disability benefit.
They class you as ‘fit to work’.
They think you are just reluctant.
You cannot go to the toilet without help. How will you go to work?

Imagine that you are lucky enough to get a specialist referral.
The nearest ME clinic is in another county.
They tell you they don’t provide services for people with severe ME anyway.
You cannot get medical help. How will you manage your illness?

This is the reality of the ME crisis.

Think of the 1 in every 263 sick.
The 62,500 housebound.
The 57% who seriously contemplate suicide.

Each icon is a person living with the cost of this crisis.
































Citations-
[1] based on data from the UK Biobank, as cited by the National Institute for Health and Care Excellence, here
[2] based on 2021 population figures from the Office of National Statistics, here
[3] Nation Institute for Health and Care Excellence, here
[4] The Health-Related Quality of Life for Patients with Myalgic Encephalomyelitis / Chronic Fatigue Syndrome (ME/CFS) Michael Falk Hvidberg ,Louise Schouborg Brinth ,Anne V. Olesen, Karin D. Petersen ,Lars Ehlers Published: July 6, 2015, here
[5] Falk Hvidberg M, Brinth LS, Olesen AV, Petersen KD, Ehlers L. The Health-Related Quality of Life for Patients with Myalgic Encephalomyelitis / Chronic Fatigue Syndrome (ME/CFS). PLoS One. 2015 Jul 6;10(7):e0132421. doi: 10.1371/journal.pone.0132421. PMID: 26147503; PMCID: PMC4492975, here
[6] De Becker, P.; McGregor, N.; De Meirleir, K. (September 15, 2001). “A definition-based analysis of symptoms in a large cohort of patients with chronic fatigue syndrome”. Journal of Internal Medicine. 250 (3): 234–240. doi:10.1046/j.1365-2796.2001.00890.x. ISSN 0954-6820, here
[7] Campen CLMV, Rowe PC, Visser FC. Reductions in Cerebral Blood Flow Can Be Provoked by Sitting in Severe Myalgic Encephalomyelitis/Chronic Fatigue Syndrome Patients. Healthcare (Basel). 2020 Oct 11;8(4):394. doi: 10.3390/healthcare8040394. PMID: 33050553; PMCID: PMC7712289., here
[8] Baxter H, Speight N, Weir W. Life-Threatening Malnutrition in Very Severe ME/CFS. Healthcare (Basel). 2021 Apr 14;9(4):459. doi: 10.3390/healthcare9040459. PMID: 33919671; PMCID: PMC8070213, here
[9] Carruthers, BM; van de Sande, MI; De Meirleir, KL; Klimas, NG; Broderick, G; Mitchell, T; Staines, D; Powles, ACP; Speight, N; Vallings, R; Bateman, L; Bell, DS; Carlo-Stella, N; Chia, J; Darragh, A; Gerken, A; Jo, D; Lewis, DP; Light, AR; Light, KC; Marshall-Gradisnik, S; McLaren-Howard, J; Mena, I; Miwa, K; Murovska, M; Stevens, SR (2012), Myalgic encephalomyelitis: Adult & Paediatric: International Consensus Primer for Medical Practitioners (PDF), ISBN 978-0-9739335-3-6, here
[10] as cited in Chu L, Elliott M, Stein E, Jason LA. Identifying and Managing Suicidality in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome. Healthcare (Basel). 2021 May 25;9(6):629. doi: 10.3390/healthcare9060629. PMID: 34070367; PMCID: PMC8227525, here
[11] Hansard, here
[12] Fennell PA, Dorr N, George SS. Elements of Suffering in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: The Experience of Loss, Grief, Stigma, and Trauma in the Severely and Very Severely Affected. Healthcare (Basel). 2021 May 9;9(5):553. doi: 10.3390/healthcare9050553. PMID: 34065069; PMCID: PMC8150911, here
[13] Anecdotal, Hansard, here
[14] De Silva RE, Bayliss K, Riste L, Chew-Graham CA. Diagnosing Chronic Fatigue Syndrome in South Asians: Lessons from a Secondary Analysis of a UK Qualitative Study. J Family Med Prim Care. 2013 Jul;2(3):277-82. doi: 10.4103/2249-4863.120765. PMID: 24479098; PMCID: PMC3902687, here
[15] Anecdotal, here
[16] Geraghty K, Jason L, Sunnquist M, Tuller D, Blease C, Adeniji C. The ‘cognitive behavioural model’ of chronic fatigue syndrome: Critique of a flawed model. Health Psychol Open. 2019 Apr 23;6(1):2055102919838907. doi: 10.1177/2055102919838907. PMID: 31041108; PMCID: PMC6482658., here
[17] Wessely S, David A, Butler S, Chalder T. Management of chronic (post-viral) fatigue syndrome. J R Coll Gen Pract. 1989 Jan;39(318):26-9. PMID: 2553945; PMCID: PMC1711569, here
[18] Green CR, Cowan P, Elk R, et al. (2015) National Institutes of Health pathways to prevention workshop: Advancing the research on myalgic encephalomyelitis/chronic fatigue syndrome. Annals of Internal Medicine 162: 860–865.
[19] Glassford JA. The Neuroinflammatory Etiopathology of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS). Front Physiol. 2017 Feb 17;8:88. doi: 10.3389/fphys.2017.00088. PMID: 28261110; PMCID: PMC5314655, here
[20] Wirth, K.J., Scheibenbogen, C. & Paul, F. An attempt to explain the neurological symptoms of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome. J Transl Med 19, 471 (2021), here
[21] NHS Inform, here
[22] Rutherford G, Manning P, Newton JL. Understanding Muscle Dysfunction in Chronic Fatigue Syndrome. J Aging Res. 2016;2016:2497348. doi: 10.1155/2016/2497348. Epub 2016 Feb 22. PMID: 26998359; PMCID: PMC4779819, here
[23] Wirth, K.J., Scheibenbogen, C. Pathophysiology of skeletal muscle disturbances in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS). J Transl Med 19, 162 (2021), here
[24] Natelson, Benjamin; Mao, Xiangling; Stegner, Aaron J; Lange, Gudrun; Vu, Diana; Blate, Michelle; Kang, Guoxin; Soto, Eli; Kapusuz, Tolga; Shungu, Dikoma C (2017). “Multimodal and simultaneous assessments of brain and spinal fluid abnormalities in chronic fatigue syndrome and the effects of psychiatric comorbidity”. Journal of the Neurological Sciences. 375: 411-416. doi:10.1016/j.jns.2017.02.046.
[25] Costa, D.C.; Tannock, C.; Brostoff, J. (November 1995). “Brainstem perfusion is impaired in chronic fatigue syndrome”. QJM: monthly journal of the Association of Physicians. 88 (11): 767–773. ISSN 1460-2725. PMID 8542261.
[26] Barnden, Leighton R.; Crouch, Benjamin; Kwiatek, Richard; Burnet, Richard; Mernone, Anacleto; Chryssidis, Steve; Scroop, Garry; Del Fante, Peter (2011). “A brain MRI study of chronic fatigue syndrome: evidence of brainstem dysfunction and altered homeostasis”. NMR in Biomedicine. 24 (10): 1302–1312. doi:10.1002/nbm.1692. ISSN 1099-1492. PMC 4369126. PMID 21560176.
[27] Hurwitz, BE; Coryell, VT; Parker, M; Martin, P; LaPerriere …., A; Bilsker, MS. “Chronic fatigue syndrome: illness severity, sedentary lifestyle, blood volume and evidence of diminished cardiac function”. Clinical Science. 118 (2): 125–135
[28] Streeten, DHP; Bell, D (1998). “Circulating Blood Volume in Chronic Fatigue Syndrome”. Journal of Chronic Fatigue Syndrome. 4: 3–11.
[29] Simpson, LO (1989), “Nondiscocytic erythrocytes in myalgic encephalomyelitis”, The New Zealand Medical Journal, 102 (864): 126–127, PMID 2927808
[30] Peterson, PK; Sirr, SA; Grammith, FC; Schenck, CH; Pheley, AM; Hu, S; Chao, C C (March 1994). “Effects of mild exercise on cytokines and cerebral blood flow in chronic fatigue syndrome patients”. Clinical and Diagnostic Laboratory Immunology. 1 (2): 222–226. ISSN 1071-412X. PMID 7496949.
[31] Logan, Alan C; Venket Rao, A; Irani, Dinaz (June 2003). “Chronic fatigue syndrome: lactic acid bacteria may be of therapeutic value”. Medical Hypotheses. 60 (6): 915–923. doi:10.1016/S0306-9877(03)00096-3. ISSN 0306-9877.
[32] Giloteaux, Ludovic; Goodrich, Julia K.; Walters, William A.; Levine, Susan M.; Ley, Ruth E.; Hanson, Maureen R. (June 23, 2016). “Reduced diversity and altered composition of the gut microbiome in individuals with myalgic encephalomyelitis/chronic fatigue syndrome”. Microbiome. 4. doi:10.1186/s40168-016-0171-4. ISSN 2049-2618. PMC 4918027. PMID 27338587.
[33] Giloteaux, Ludovic; Goodrich, Julia K.; Walters, William A.; Levine, Susan M.; Ley, Ruth E.; Hanson, Maureen R. (June 23, 2016). “Reduced diversity and altered composition of the gut microbiome in individuals with myalgic encephalomyelitis/chronic fatigue syndrome”. Microbiome. 4. doi:10.1186/s40168-016-0171-4. ISSN 2049-2618. PMC 4918027. PMID 27338587.
[34] Maes, Michael; Mihaylova, Ivana; Leunis, Jean-Claude (April 1, 2007). “Increased serum IgA and IgM against LPS of enterobacteria in chronic fatigue syndrome (CFS): Indication for the involvement of gram-negative enterobacteria in the etiology of CFS and for the presence of an increased gut–intestinal permeability”. Journal of Affective Disorders. 99 (1): 237–240. doi:10.1016/j.jad.2006.08.021. ISSN 0165-0327.
[35] Tomas, Cara; Newton, Julia (June 19, 2018). “Metabolic abnormalities in chronic fatigue syndrome/myalgic encephalomyelitis: a mini-review”. Biochemical Society Transactions. 46 (3): 547–553. doi:10.1042/BST20170503. ISSN 0300-5127.
[36] Sweetman, Eiren; Kleffmann, Torsten; Edgar, Christina; de Lange, Michel; Vallings, Rosamund; Tate, Warren (September 24, 2020). “A SWATH-MS analysis of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome peripheral blood mononuclear cell proteomes reveals mitochondrial dysfunction”. Journal of Translational Medicine. 18 (1): 365. doi:10.1186/s12967-020-02533-3. ISSN 1479-5876. PMC 7512220.
[37] Armstrong, Christopher W.; McGregor, Neil R.; Lewis, Donald P.; Butt, Henry L.; Gooley, Paul R. (May 30, 2015). “Metabolic profiling reveals anomalous energy metabolism and oxidative stress pathways in chronic fatigue syndrome patients”. Metabolomics. 11 (6): 1626–1639. doi:10.1007/s11306-015-0816-5. ISSN 1573-3882.
[38] Naviaux, Robert K.; Naviaux, Jane C.; Li, Kefeng; Bright, A. Taylor; Alaynick, William A.; Wang, Lin; Baxter, Asha; Nathan, Neil; Anderson, Wayne (September 13, 2016). “Metabolic features of chronic fatigue syndrome”. Proceedings of the National Academy of Sciences. 113 (37): E5472–E5480. doi:10.1073/pnas.1607571113. ISSN 0027-8424. PMID 27573827
[39] based on data from the ME Association, as cited here
[40] BBC News, here